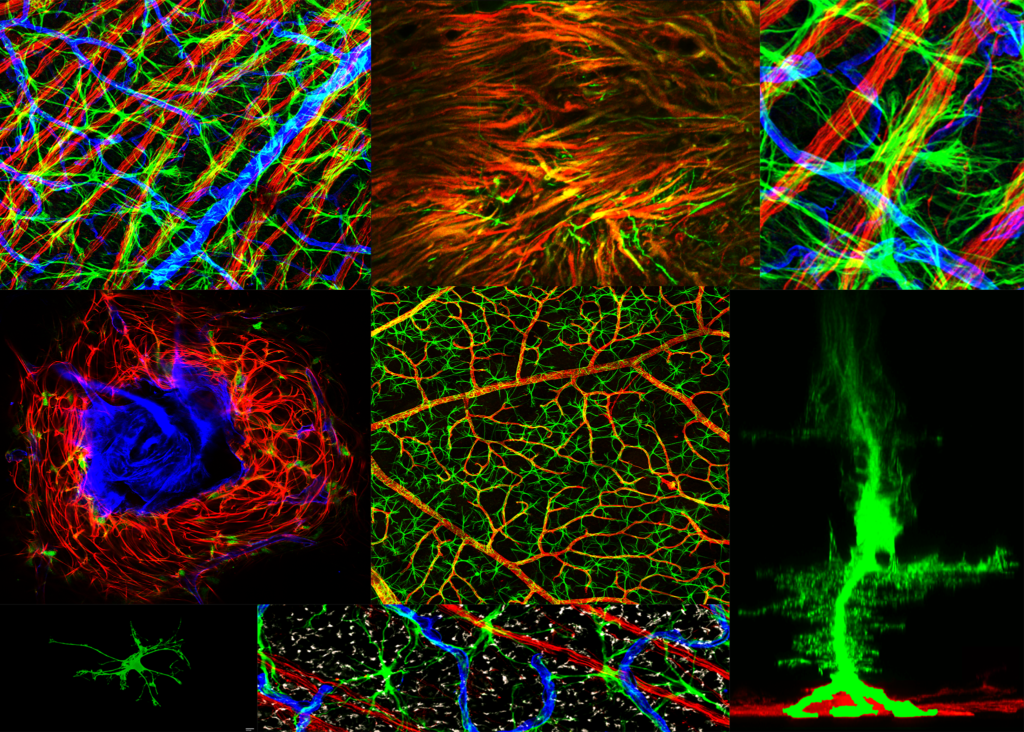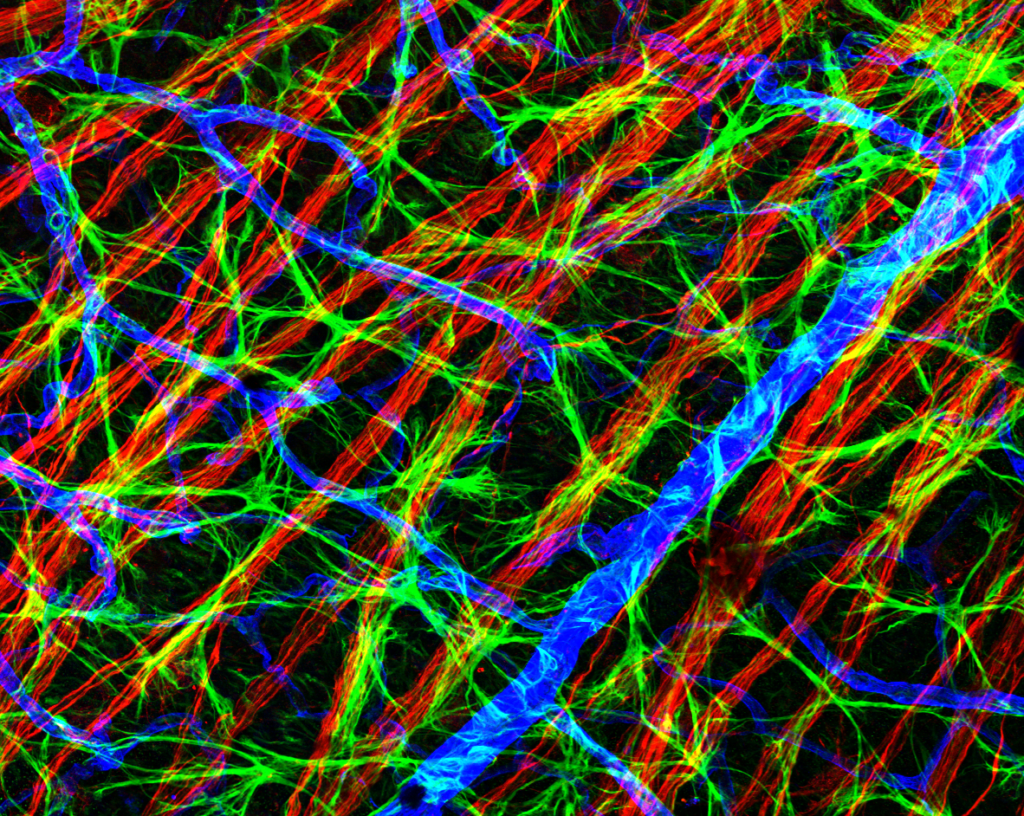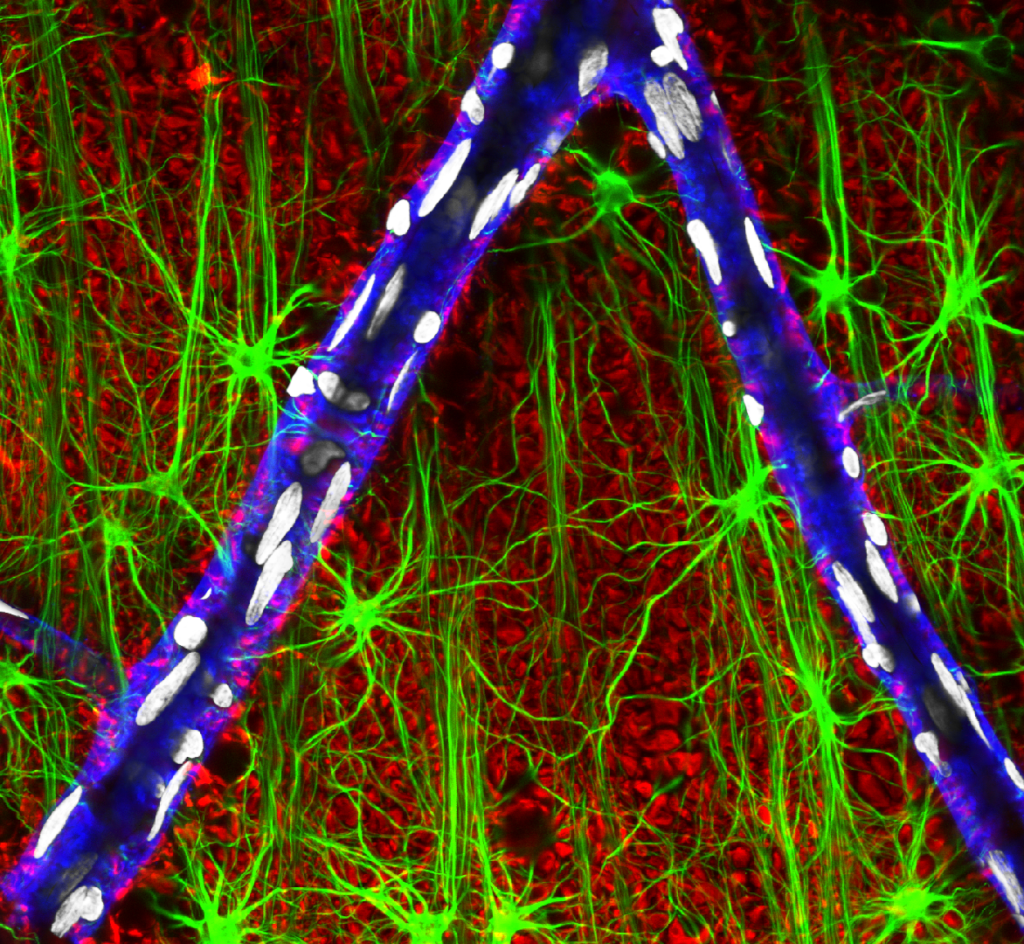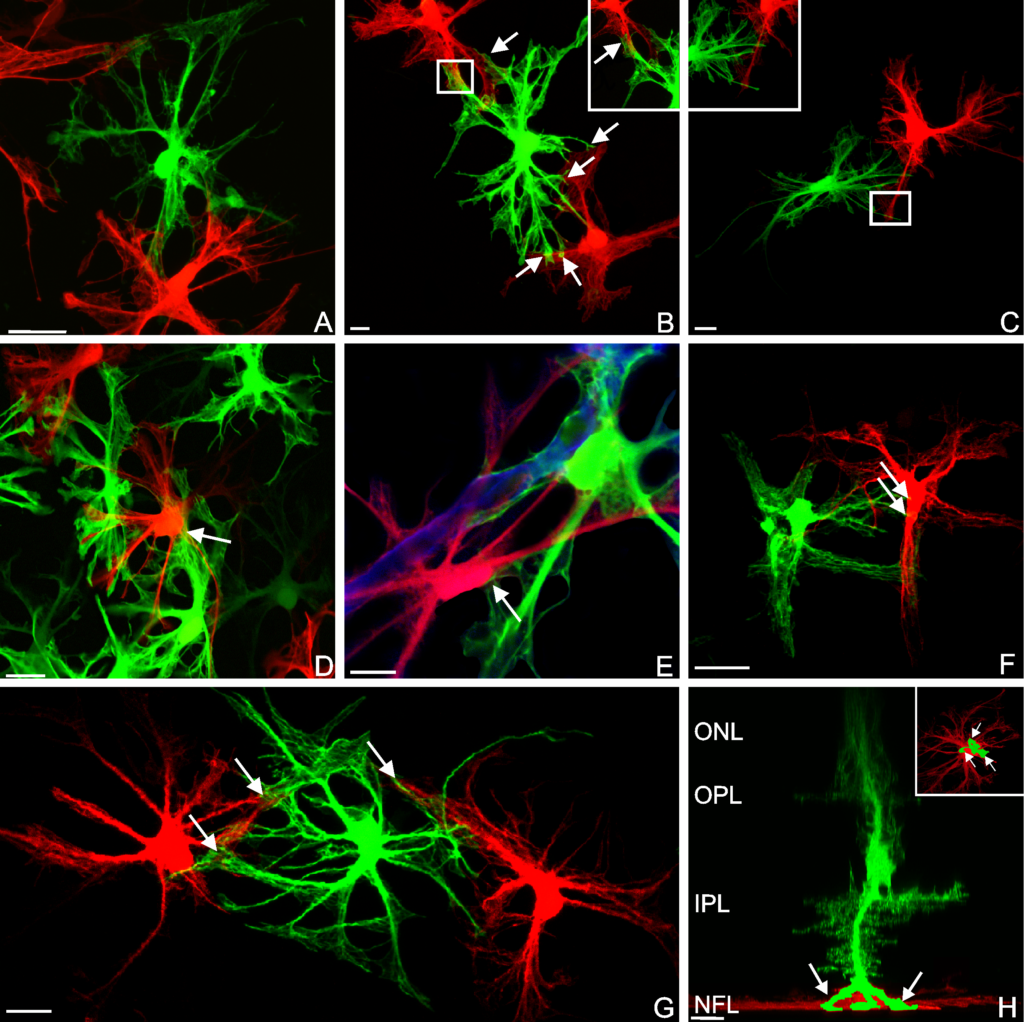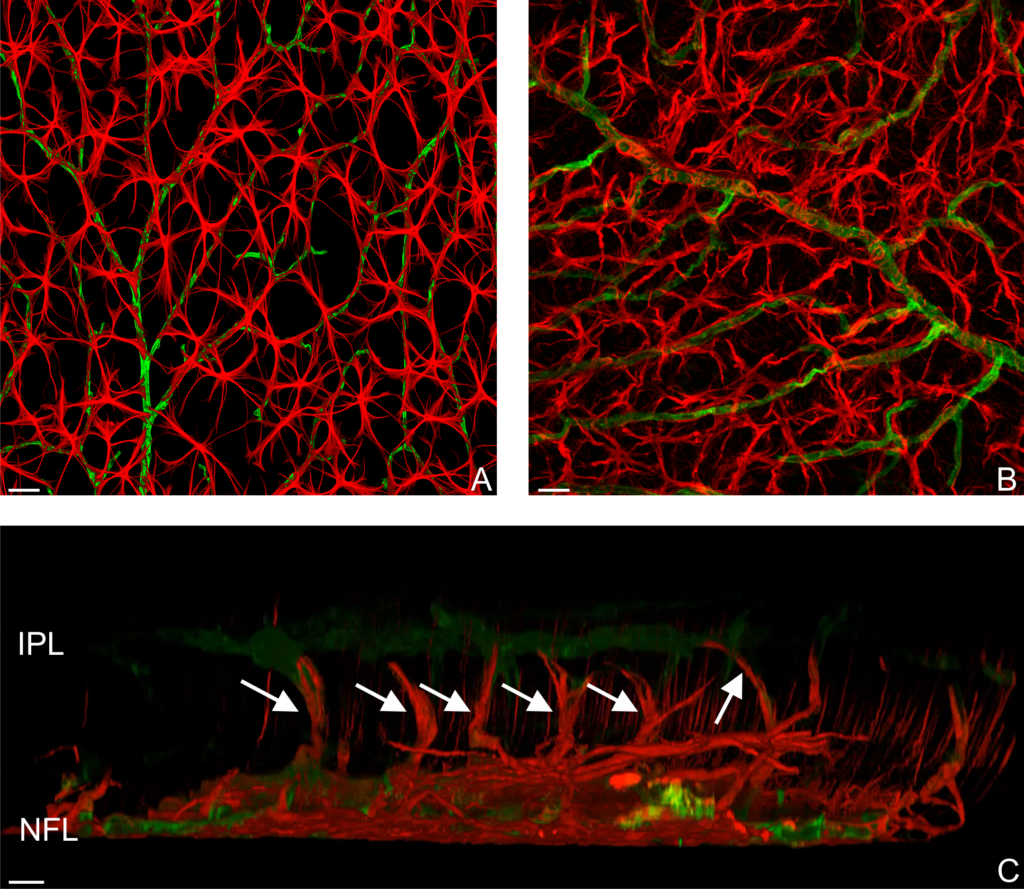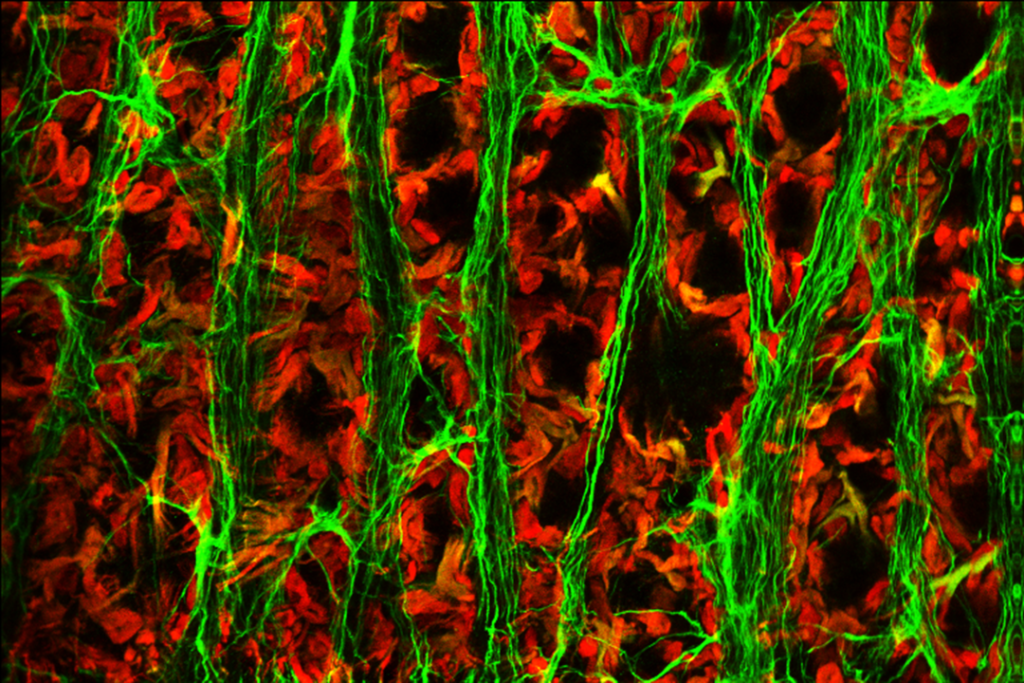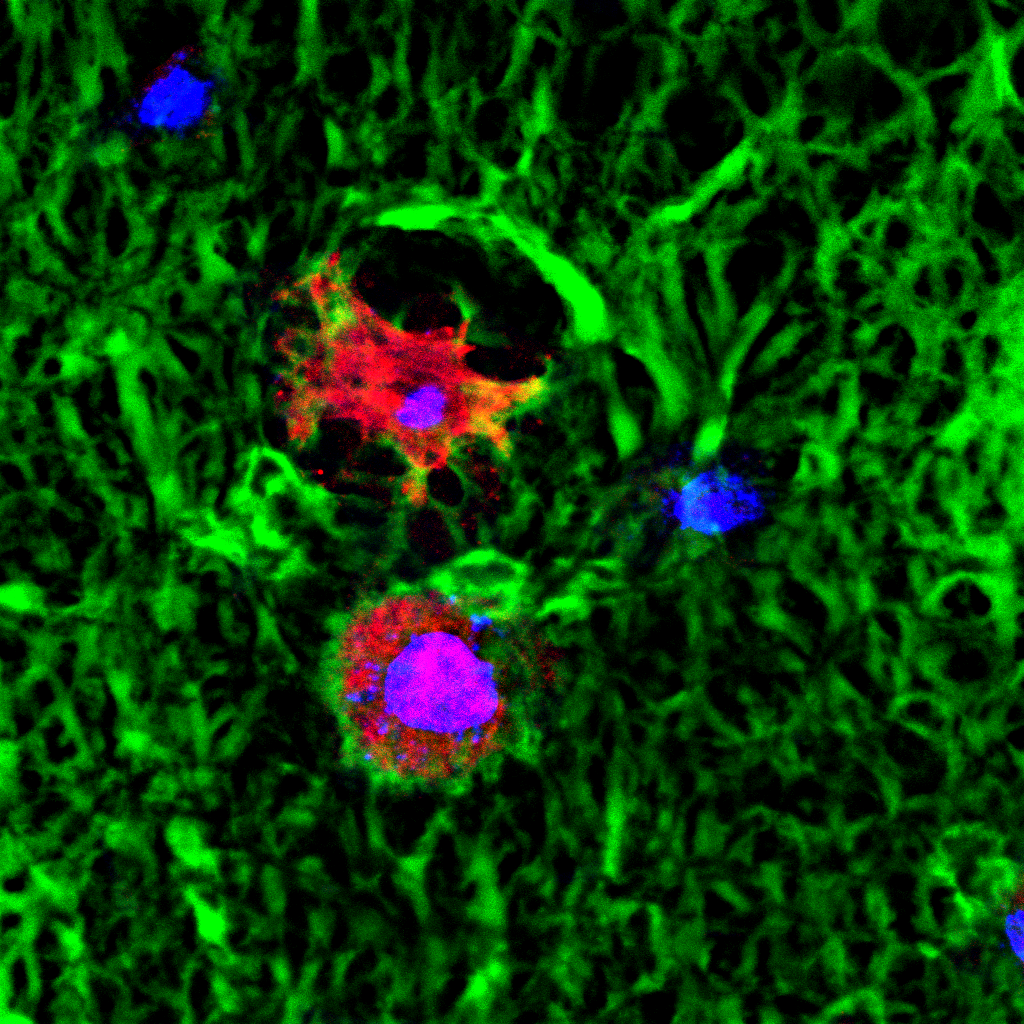
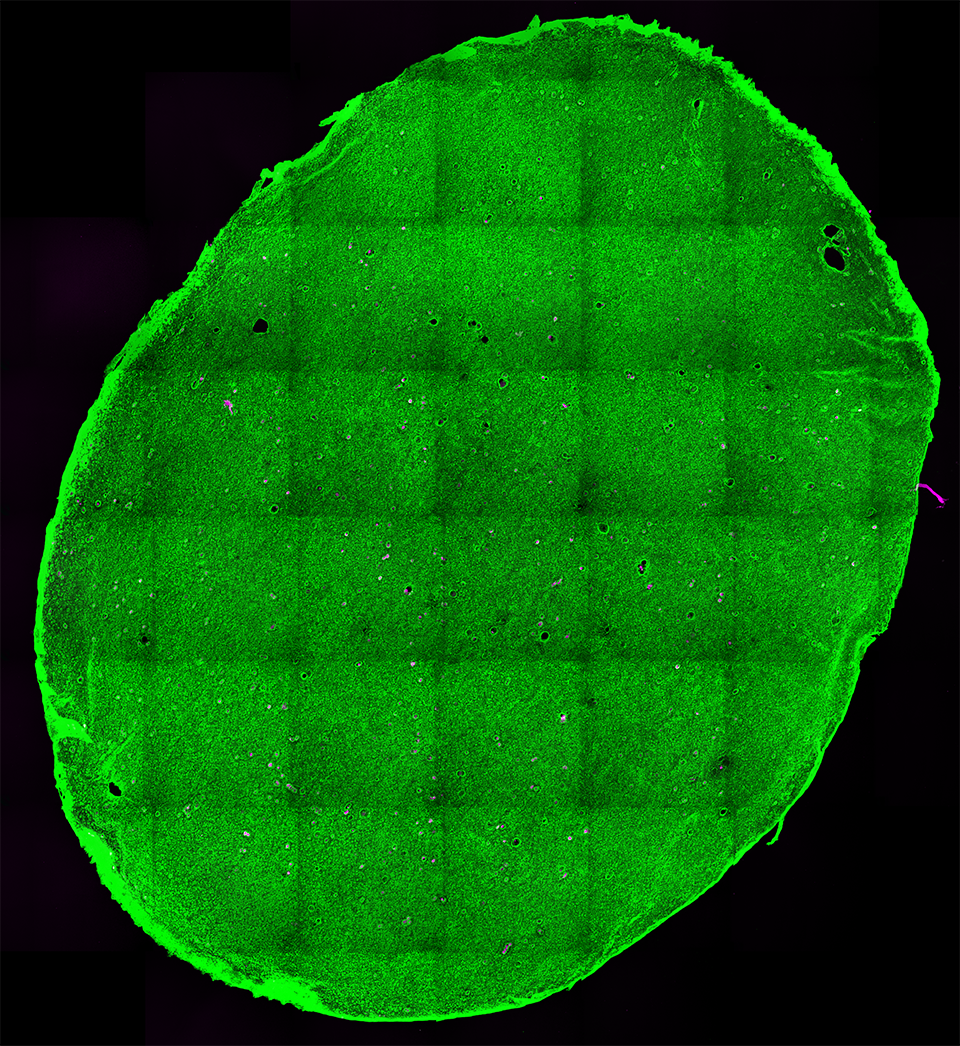
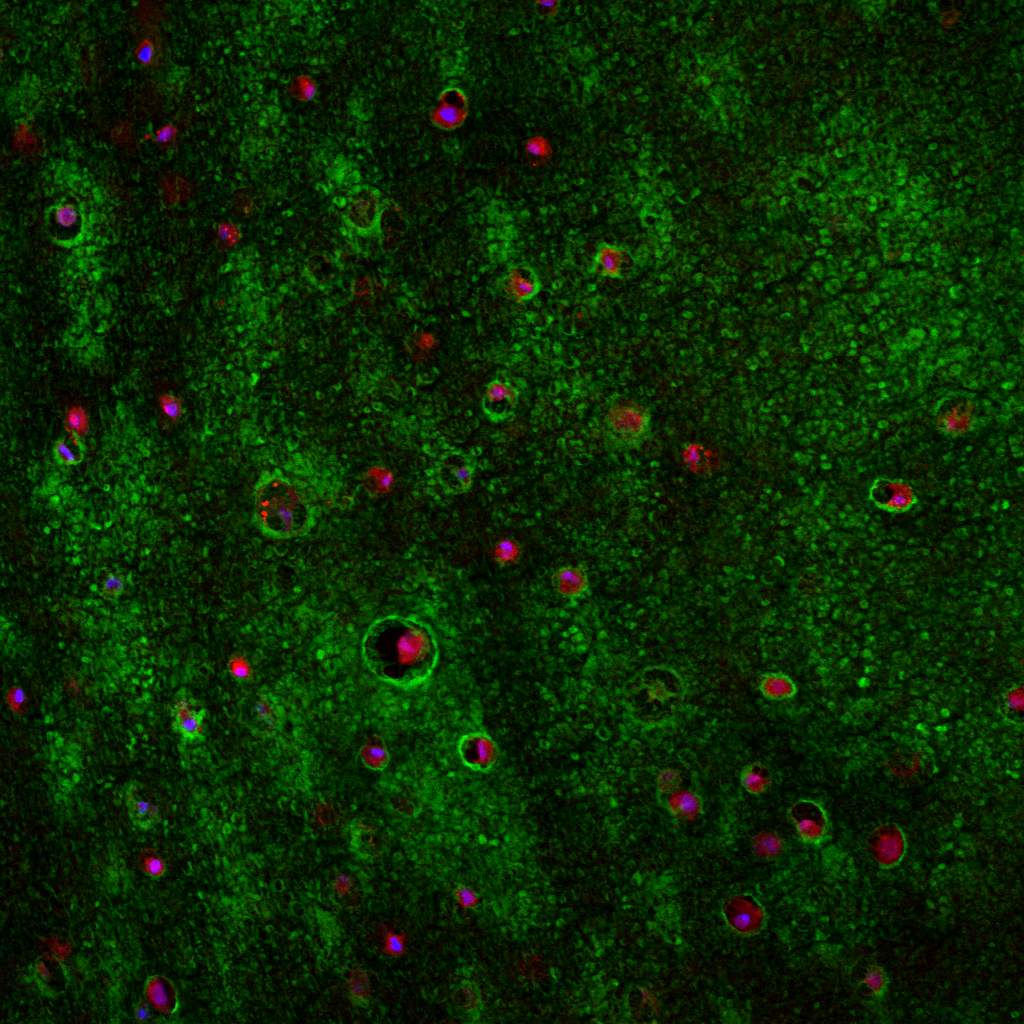
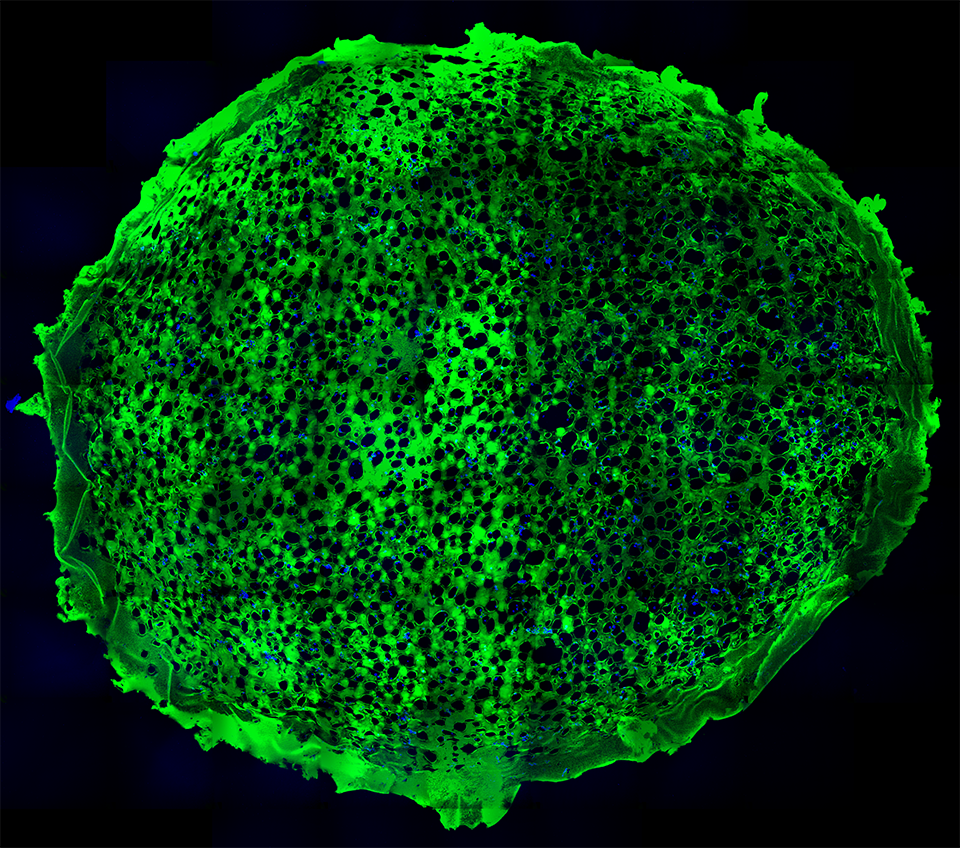
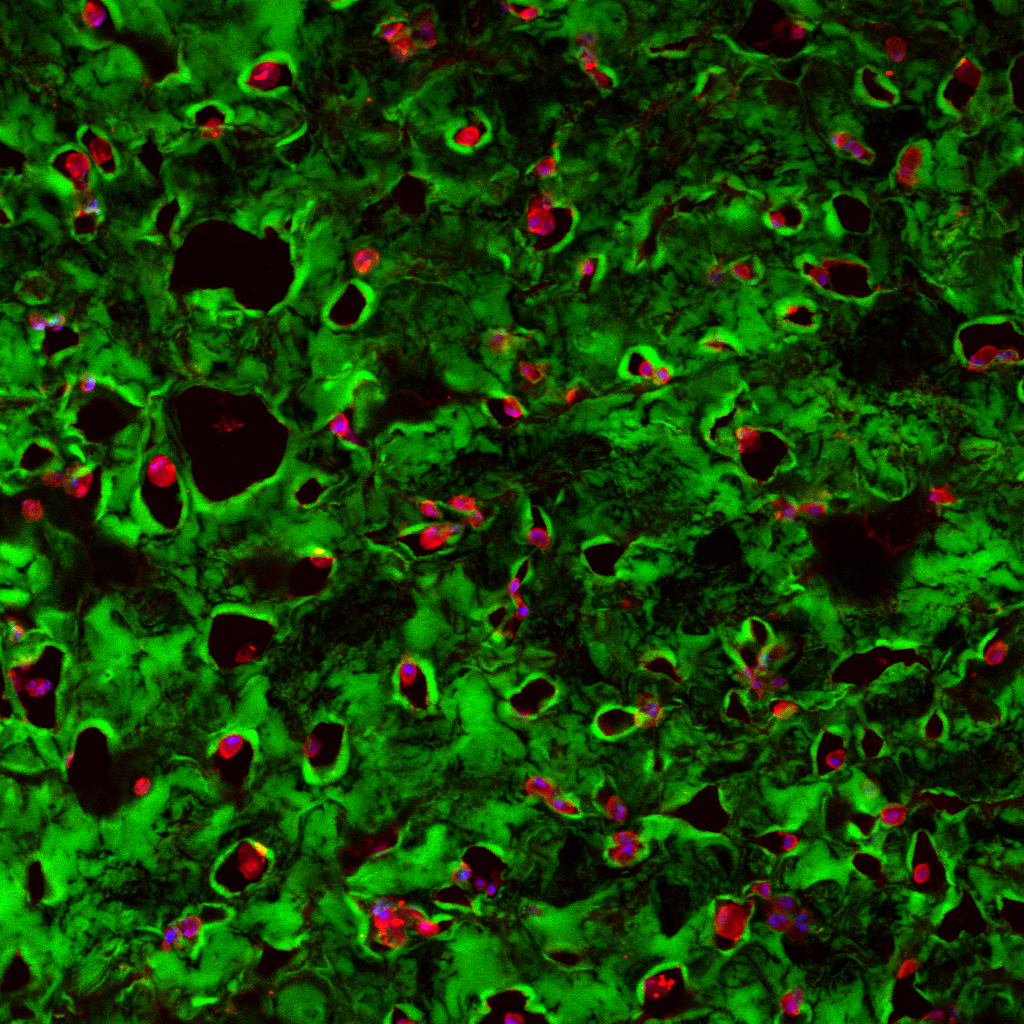


New publication! Drs. Tracy Clevenger, Steve Fisher, Dennis Clegg and myself recently reviewed wide-ranging strategies concerning synthetic scaffolds and their potential to foster adipose-derived stem cells as therapies involving soft-tissue, bone, and cartilage, that work can be found here. Research involving adipose-derived stem cells has potential implications in a wide-range of applications encompassing cosmetic procedures, burn patients, and wound healing, however, research involving these cells remains in its infancy. Microscopy images above show examples of these synthetic systems harboring stem cells, in these images the green color corresponds to the synthetic scaffold, the blue indicates the nucleus of an individual adipose-derived stem cell, lastly the red displays a part of the cells’ cytoskeleton that in part reveals its “shape”.
Abstract: Regenerative medicine possesses the potential to ameliorate damage to tissue that results from a vast range of conditions, including traumatic injury, tumor resection and inherited tissue defects. Adult stem cells, while more limited in their potential than pluripotent stem cells, are still capable of differentiating into numerous lineages and provide feasible allogeneic and autologous treatment options for many conditions. Adipose stem cells are one of the most abundant types of stem cell in the adult human. Here, we review recent advances in the development of synthetic scaffolding systems used in concert with adipose stem cells and assess their potential use for clinical applications.